The home can be a dangerous place for the person with Alzheimer’s. They spend many hours in the living room, so addressing Alzheimer’s Disease living room safety is crucial.
The living areas, such as living rooms and dens, should be safe and comfortable gathering places for families. The person with dementia needs to feel part of the family and the rooms must accommodate his or her needs.

Read this article as a guide and then print off the checklist below to use as you go through your home’s living areas looking for dangers.
Alzheimer’s Disease Living Area Safety Checklist (PDF)
Step One: Focus on the Space Itself
Make sure the living area has plenty of space to roam with clear pathways. This may require getting rid of some of the furniture, such as extra chairs, side tables, and bookcases. First, look for the furniture that might be removed for its danger factor.
- Moreover, remove anything that obstructs a clear path. This includes foot stools and furniture.
- Reduce clutter. Too much clutter can cause confusion and agitation. Remove as much clutter as possible to make the space roomier. Trash cans, statues, and floor lamps can be in the way and serve as trip hazards. Stacks of magazines and newspapers can be overwhelming.
Step Two: Look at Your Furniture
Look at the furniture for usability and safety.
- Address sharp edges. Is there furniture with sharp edges that could pose a danger? If so, can you live without them in order to make the room more spacious and safe? If not, consider padding the edges. There are low-cost products to help with this.
- Get rid of wobbly furniture. If your loved one leans on the furniture, it needs to support him or her. Furniture with glass that could be easily broken should be removed.
- Seating should be firm and sturdy. Do chairs have arms for the older person to hold onto when getting up? If the seat needs to be higher, consider adding a firm cushion to the chair for added height.
- Protect upholstery from spills. Use a heavy-duty substance, such as Scotchgard. Alternatively, use slipcovers to protect expensive furniture.
- Rolling chairs should be removed. Consider removing rocking chairs, too. They are not the best choice for a person with balance issues. Still, a rocking chair is something older people often use in their own homes, and the rocking action is generally soothing. Some rocking chairs are safer than others, so you don’t have to rule them out.
- Look into getting a lift chair if needed. Your loved one may be used to relaxing in a recliner. If this is the case, but getting up from one is a problem, the power lift chair may be your answer. You can buy a regular chair and order the lifting apparatus to attach to it. Check with the doctor for a recommendation. Medicare may pay for the attachable lifting mechanism.
- Check tables for sturdiness. Do end tables serve a purpose? Are they steady to the touch? Would they hold up if someone held onto them to prevent falling? If the answer to these questions is no, then you might need to remove them from the room.
- Footstools and coffee tables pose a potential tripping hazard. In addition, the person with dementia, not realizing how low the stools are to the ground, might sit on one and fall off or not be able to get back up. A contrasting color to the carpet will reduce the threat as a tripping hazard. Depending on the material of the table or stool, you could paint it to better contrast with the color of the carpet in order for the table to be easily spotted.
Step Three: Focus on Decorations
Decorations need to be addressed both in terms of safety and for comfort. You should remove any items that pose a threat yet leave items that make your loved one feel at home.
- Keep favorite items to make the room familiar and homey. Things that are familiar might be a clock or a particular painting. Does he or she have favorite knick-knacks or collections?
- Locking breakable items in a display case is an option. If it gets to the point where seeing a prized collection but not being able to get to it becomes distressing, then it might be time to store the items out of sight. For the person with dementia, out of sight may be out of mind.
- Look for heavy decorations that might be positioned throughout the room. Bookends? Free-standing clocks? What about heavy books with prominent edges? Any of these items could become dangerous if the person with dementia were to become agitated and throw one in a fit of anger. Evaluate every item in the living room and throughout the house.
- Never light candles in a home where someone with dementia roams. If you enjoy the inviting warmth of candles, there are battery-powered candles that mimic the mood of real candles.
- Remove any plants that could be toxic if eaten. Check a list of plants that fall in this category, either online or by calling the Poison Control Center. Also, remove any small stones in the base of the pot, as they could be picked up and put in the mouth.
- Remove any items with openings as such that could be perceived as a toilet. Just as in the bathroom, or in any room, certain objects can be mistaken for a toilet. Flower pots are one of those items, as are magazine holders and umbrella stands.
Step Four: Assess Lighting and Fans
As in any room, the living room should be well-lit with bright bulbs overhead. If you must use table lamps, make sure the cords are out of the way. Long cords or extension cords can be tacked to the baseboards to keep them from being a trip hazard.
- In lamps, replace incandescent bulbs with fluorescent. Fluorescent bulbs won’t get as hot to the touch should wandering hands land on them.
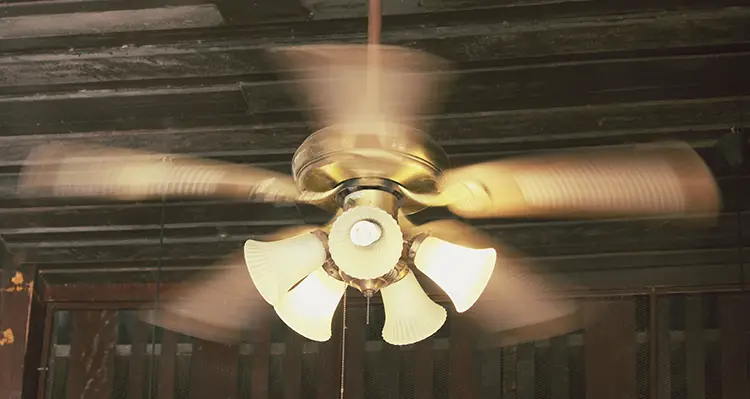
- Lighting is affected by ceiling fans. Check to see if the fan makes the light “jump” and throw shadows. Either can be distracting and irritating to a person with dementia.
- Check ceiling fans for other factors. Are they too low or too loose? Are they too loud? Loudnoise is yet another assault on the senses that causes irritation. Even the draft from a fan, or “wind” perceived by the person with dementia, may be unsettling and uncomfortable to someone with altered perception.
- Close blinds and curtains at dark. As daylight fades, windows and sliding glass doors will operate as mirrors by bouncing back the reflection of the onlooker.
Step Five: Don’t Forget Potential Exits
Speaking of sliding glass doors, during the day, these glass doors may invite a person to wander out into the yard or garden. You must ensure that your loved one does not wander outside alone.
- Make sure sliding glass doors or other exits are locked. Locks can be installed up high or down low or both, making opening those more of a challenge. There are also low-cost door alarms that can be installed to notify you if they are opened.
- Camouflaged exits keep the wanderer from recognizing the door as an exit. In some dementia units within long-term care facilities, they hire an artist to paint a scene on exit doors that blends the door with the rest of the room, completely masking the appearance of an exit. This type of alteration may be too drastic for the look of your home, and it may cost more than what you are willing or able to pay. This practice, however, has been known to work in nursing homes. A lower-cost option may be painting the door the same color as the wall.
- Doorknob covers also prevent egress. These low-cost covers can be found in the baby section of most department stores. They make turning the knob more of a challenge.
Step Six: Additional Tips
Depending on the needs of your loved one and the space in which you reside, you may need to implement some or all of the following suggestions. Use these to guide you through necessary changes.
- Look at drapes or curtains. While curtains make a room appear homier, those with busy prints can be irritating to the person with Alzheimer’s. Opt for solid colors for your curtains throughout the house.
- If curtains are too long and could be tripped over, they should be shortened. You might pull the curtains themselves back, while letting the blinds do the job of covering the windows after the sun goes down.
- Purchase cord-safe products to shorten cords on blinds. It seems there are potential dangers everywhere you turn, as the blinds present yet another hazard with the cord that hangs down. Avoid the temptation for anyone to want to play with the cord, or, worse, to get wrapped up in it. These provide an out-of-the-way place to wrap cords and keep them from dangling.
- Make sure carpeting is secure and smooth. An individual with dementia scoots his or her feet and can thus stumble over ripples in the carpet. Likewise, area rugs, since they are not flush with the floor, can present a tripping hazard. Have you ever seen area rugs in a nursing home resident’s room? There is a reason for that.
- Hardwood floors can be dangerous if they are not level. This may be a problem in older homes. Remember that hardwood floors should not be too shiny or easily slid on.
- Prevent accidents before they happen. Look around to see what could be a danger. Cover the fireplace with a protective guard. Attach padding to the edges. Are you afraid of your flat-screen TV getting knocked over? Secure it with safety straps. If you are afraid of your loved trying to climb a bookcase or tipping over another heavy piece of furniture, tie it down.
- Control the noise. A lot of people keep the television on for much of the day. Noise is an irritant to someone with dementia and can encourage agitation or aggression, thus spurring on efforts to leave the area. Instead of playing the TV, try soothing music for your loved one. Don’t leave anything—even music—playing all the time, though, as constant stimulation can bring on agitation as well. Similarly, if you have a home telephone, turn down the ringer volume to minimize confusion and keep the person with Alzheimer’s from trying to answer the phone.

After Addressing Alzheimer’s Disease Living Room Safety
This is the fourth article in this series. Further articles will cover other rooms:
- General Home Safety
- Bedroom Safety
- Bathroom Room Safety
- Kitchen Safety
- Hallways and Entryways
- Outside the Home
Check each of these articles as they become published to continue your home safety assessment.
Want to read my complete guide? See my book Staying Home.
- Grant, Derrick (Author)
- English (Publication Language)



