Palliative care may be part of the conversation when considering end-of-life care, medical treatment options, and what is important to you and your family. Confusion about palliative care is understandable – when to start and how it differs from hospice. Hospice receives much more attention, and as valuable as hospice is, palliative care plays a significant role in providing symptom relief, comfort, and support to people living with serious illnesses.
We will explore the philosophy of palliative care, how to request it, and what you can expect in the 5 stages of palliative care treatment. After all, it is your life, and you should have choices about what quality of life means to you when coping with a serious medical condition.
What is the difference between Palliative Care and Hospice Care?
People in palliative care can and usually do eventually choose hospice, but the two services, although overlapping in philosophies, are quite different.
Palliative Care
- Palliative care aims to improve the quality of life of patients and their families who are facing problems associated with life-threatening or incurable illnesses. Palliative care can last weeks or years. A terminal diagnosis is not required.
- The palliative care team comprises doctors, nurses, therapists, social workers, counselors, and volunteers.
- Palliative care alleviates suffering from pain and discomfort by addressing co-occurring physical, social, or spiritual symptoms.
- To qualify for palliative care, you do not have to have 6 months to live even though your illness may be terminal.
- Palliative care uses a team approach to support patients and their caregivers. The team works with the patient to identify what quality of life means to them and their goals of care. Living as actively as possible with chronic illness is a common goal of palliative care.
- You can receive palliative care while also receiving curative treatment for your illness.
- Palliative care services are comprehensive and holistic. For example, the palliative care team might assist you with insurance forms, nutrition, housing options, filling out advance directives, or coordinating spiritual support.
- Palliative care is covered by most insurance, but coverage may vary depending on your policy.
Hospice Care
Hospice is truly end-of-life care, although it is not rare for people to go on and off hospice for years. But the criteria for hospice and delivery of services are different from palliative care. You might think of hospice care as a type of palliative care.
- A physician must certify that your terminal condition will likely end your life within 6 months.
- Hospice care is also delivered by a team of nurses, aides, spiritual personnel, volunteers and doctors.
- You cannot receive curative treatment for the condition that qualifies you for hospice. However, other treatment related to comfort is acceptable. For example, antibiotics for an infection, oxygen for respiratory problems, high blood pressure medication, etc.
- Hospice care focuses on pain and symptom management, emotional support for the patient and family, provision of medical supplies, and grief counseling. Under Medicare, hospice must provide 24-hour on-call support for emergencies. But, hospice does not provide round-the-clock care.
When should someone be offered Palliative Care?
You can request palliative care at any time following a serious medical diagnosis. Examples of conditions where palliative care is most often used are chronic obstructive pulmonary disease, cancer, dementia or Alzheimer’s disease, neurological diseases, Parkinson’s disease, ALS, kidney disease, etc. You don’t need to be near death to qualify for palliative care.
Everyone is different, but some of the signs that it might be time to consider palliative care are:
- You have been diagnosed with a chronic medical condition requiring monitoring and treatment
- Frequent emergency room visits and doctors appointments are exhausting
- You are having trouble coping with pain and discomfort related to your condition
- You need additional emotional, physical, and spiritual support
- You would like to have as much quality of life as possible while living with your disease but need more support and guidance to make that happen.
- Family caregiver burnout and stress are increasing your anxiety about your care.
If you are in doubt about whether you want palliative care, talk with your primary care physician about the pros and cons of such a decision. Even if you start palliative care, you can change your mind later.
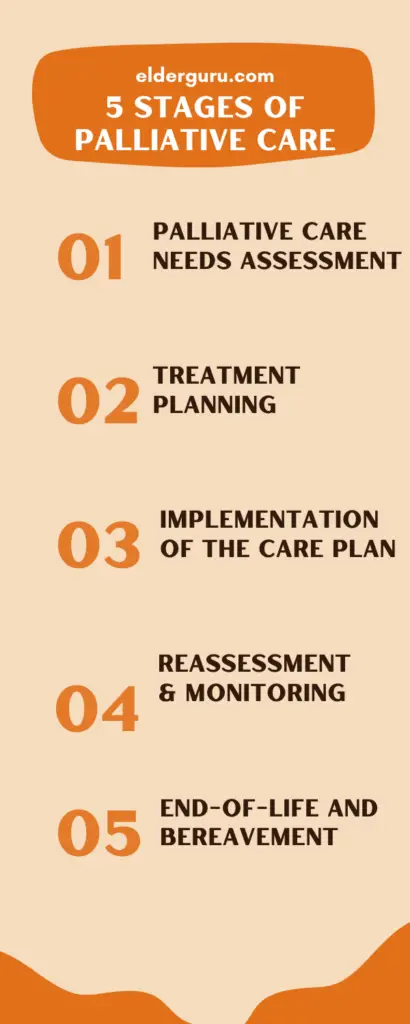
What are the 5 stages of Palliative Care?
On a practical level, what is it like to receive palliative care, and what is the process? These stages differ depending on the team you have or the nature of your illness, but generally, there are 5 stages of palliative care. With chronic illness, there is an expected process of deterioration, but that does not occur in all cases. You may not go through these stages in a particular order as your condition changes.
Stage 1: Palliative care needs assessment (Stable)
In this stage, palliative care team members assess your needs, goals, and preferences. Assessment is comprehensive and could include:
- Prognosis and current treatment regime.
- Medications and efficacy of pain relief
- Your current and future treatment plan
- The expected progression of your illness
- Care preferences and wishes including specific circumstances where you may not want resuscitation or continued treatment. Also, you would create advance directives at this stage if you haven’t already done so.
Stage 2: Treatment planning
The palliative care team develops a personalized, individualized care plan. The care plan is flexible due to the changing nature of medical conditions and guides the team as they work to meet your goals.
Stage 3: Implementation of the care plan (potential for instability)
During this stage, the care plan is put into action. The agreed-upon medical interventions, pain management, and symptom control are implemented. Emotional and psychological support is provided to you and your family. Coordination between healthcare professionals and collaboration with your primary care provider is emphasized.
Every chronic medical condition has a different trajectory, and the potential for instability is expected. There will be ups and downs.
Stage 4: Continual reassessment and monitoring: (potential for deterioration)
Palliative care is dynamic, and your needs may change over time. Regular reassessment and monitoring are crucial to ensure that the care plan remains effective. Adjustments are implemented as symptoms and care needs change.
As a patient, you may want to change your approach to pain management as you worsen, or you could decide to end many of the treatments you started. The choices are yours.
Stage 5: End-of-life and bereavement support (Terminal)
In the final stage, palliative care transitions to bereavement support if the patient dies. The focus shifts to helping the patient’s loved ones cope with grief and loss. Emotional support, counseling, and practical assistance may be provided to the family during this difficult time.
The terminal stage, also called the “end of life” stage, signifies that death may be imminent within days. At this point, hospice may be initiated, or you can remain with the palliative care team. You may become bedridden or experience mobility issues. Some common symptoms at the end of life are:
- Fatigue
- Loss of interest in food or drink
- An increase in pain and physical and emotional discomfort
- Talking less and sleeping more
- Possible anxiety and fear about dying
- A transition to comfort care only
When a patient dies, the palliative care team provides spiritual support for the family and counseling for grief and loss.
Where is Palliative Care offered?
Palliative care can be provided wherever the patient is. This includes nursing homes, residential homes, assisted living, memory care, outpatient clinics, and hospitals. Veterans may be eligible for palliative care through the Department of Veterans Affairs.
Palliative Care is Underutilized
According to the World Health Organization, only about 14% of people who need palliative care receive it even though palliative care reduces hospital admissions and suffering. As our aging population grows, the value and need for palliative care will grow. Family caregivers also benefit from palliative care, receiving much-needed support and relief.
Barriers to palliative care include a lack of specialty training required, financial barriers and attitudes, and misunderstandings about the benefits. Not every community or healthcare setting will offer palliative care. But, if you are suffering from a chronic illness, and live in an area where it is offered, consider taking advantage of this valuable support service.
Frequently Asked Questions (FAQs)
-
What is the difference between palliative care and hospice?
Hospice requires a doctor’s order stating you have a terminal condition with a life expectancy of 6 months. You can start palliative care anytime; a terminal diagnosis is not required.
-
How do I know if I would benefit from palliative care?
Talk to your doctor and family members about the possibility of palliative care to help you manage a serious illness. Weigh the pros and cons and evaluate your goals of care.
-
Why are there stages of palliative care?
The stages of palliative care acquaint you with the process you can expect when you start palliative care. The stages also help to guide your palliative care team.
-
Does insurance cover palliative care?
Most insurance plans, including Medicare and Medicaid, pay for palliative care, but coverage could vary, so check with your plan.
ABOUT THE AUTHOR

Amanda Lambert is an Aging Life Care Professional and consultant with over twenty years of experience in the elder care field. She has worked in home health, mental health, and guardianship. She is a Care Manager Certified, Aging Life Care Professional, Master Guardian Emeritus, and holds a Master’s Degree from the University of Utah. Amanda also sits on the state board of AARP.